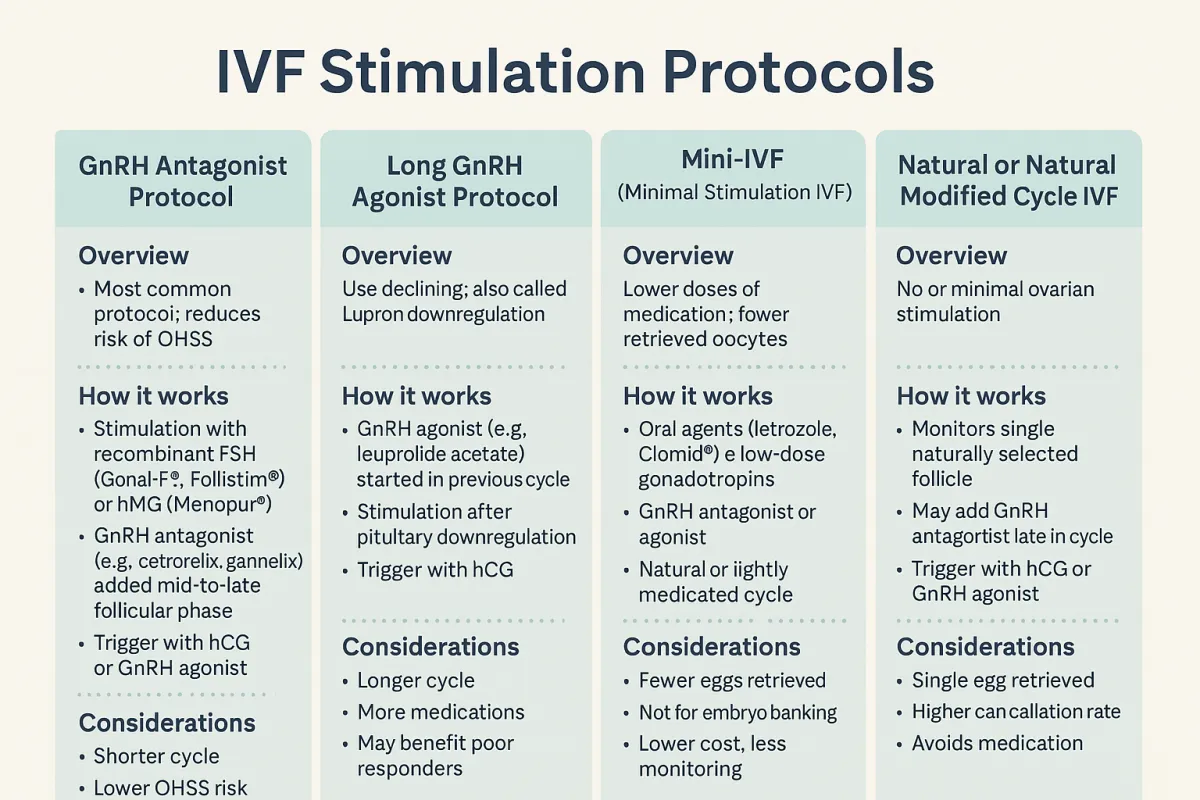
IVF Stimulation Protocols – Choosing the Right Approach
In modern IVF, ovarian stimulation is not one-size-fits-all. A variety of protocols are used based on age, ovarian reserve, past response, hormone levels, and individual goals. Here’s a breakdown of the most widely used stimulation strategies.
1. GnRH Antagonist Protocol (Flexible or Fixed Start)
Overview:
Now the most common IVF stimulation protocol in the U.S., the antagonist protocol is appreciated for its flexibility and reduced risk of ovarian hyperstimulation syndrome (OHSS).
How it works:
Stimulation begins: Day 2 or 3 of cycle with recombinant FSH (Gonal-F®, Follistim®) or hMG (Menopur®).
GnRH antagonist (e.g., cetrorelix, ganirelix) is introduced on day 5–6 or when the lead follicle reaches ~14 mm.
Trigger: Final maturation is triggered with either hCG (Pregnyl®, Ovidrel®) or a GnRH agonist (e.g., Lupron®) in high responders.
Advantages:
Shorter cycle length
Lower OHSS risk
Preferred in PCOS patients and egg donors
2. Long GnRH Agonist Protocol (Lupron Downregulation)
Overview:
Once the standard protocol, now used selectively—often for endometriosis or poor responders.
How it works:
GnRH agonist (e.g., leuprolide acetate): Started in the mid-luteal phase of the cycle prior to stimulation to suppress natural hormone fluctuations.
Stimulation begins after full pituitary downregulation (~10–14 days).
Trigger: Typically hCG.
Advantages:
More synchronized follicular growth
May improve implantation rates in specific subgroups
Drawbacks:
Longer and more intense
Risk of over-suppression in some patients
3. Mini-IVF (Minimal Stimulation IVF)
Overview:
Uses lower doses of medication with the goal of retrieving fewer, higher-quality eggs.
How it works:
Oral agents like letrozole or Clomid®, sometimes paired with low-dose gonadotropins
GnRH antagonist or agonist used for suppression
Often used in natural or lightly medicated cycles
Ideal for:
Poor responders
Older patients
Patients seeking lower-cost or lower-risk cycles
Limitations:
Fewer eggs retrieved
Not ideal for embryo banking
4. Natural or Natural Modified Cycle IVF
Overview:
No ovarian stimulation or very minimal drug use. Monitors and retrieves the single naturally selected follicle.
How it works:
Monitoring via ultrasound and labs
Possible use of GnRH antagonist late in the cycle
Trigger with hCG or GnRH agonist
Used when:
Avoiding medications
High risk for OHSS
Specific religious/philosophical beliefs
Limitations:
Single egg retrieval
Higher cycle cancellation rate
Tailoring the Protocol
Your reproductive endocrinologist chooses the protocol based on:
Antral follicle count (AFC) and AMH levels
Age and previous IVF response
Diagnosis (e.g., PCOS, diminished ovarian reserve)
Risk of OHSS
Patient preference and treatment goals