Embryo Freezing, Selection, and Single Embryo Transfer in IVF
🔹 Embryo Freezing (Cryopreservation)
Embryo freezing has shifted from a backup plan to a mainstream strategy. Today, nearly all embryos are frozen (vitrified) at the blastocyst stage, especially in clinics prioritizing frozen embryo transfer (FET) for improved uterine receptivity and safety.
✅ Why Freeze Embryos?
Time for genetic testing (PGT-A)
Reduce risk of OHSS by delaying transfer
Allow uterus to recover after stimulation
Bank embryos for future use
🔬 Vitrification vs. Slow Freezing:
Vitrification: Ultra-rapid freezing that prevents ice crystal formation → higher survival rates.
Slow Freezing: Older method, mostly phased out.
Success rates with FET now often exceed fresh transfer success due to improved protocols and timing.
🔹 Elective Single Embryo Transfer (eSET)
eSET is the standard recommendation for many patients under 35 or those with good-quality embryos. The goal is to reduce twin or triplet pregnancies, which carry higher risks for mother and babies.
🔍 When eSET is Recommended:
Age < 38
High-quality day 5 blastocysts available
First or second IVF cycle
Normal uterus and no history of failed transfers
⚖️ Benefits of eSET:
Lower risk of preterm birth, low birth weight, and preeclampsia
Comparable cumulative live birth rates with sequential FETs
🔹 Embryo Grading
Grading helps embryologists select embryos with the highest chance of implanting.
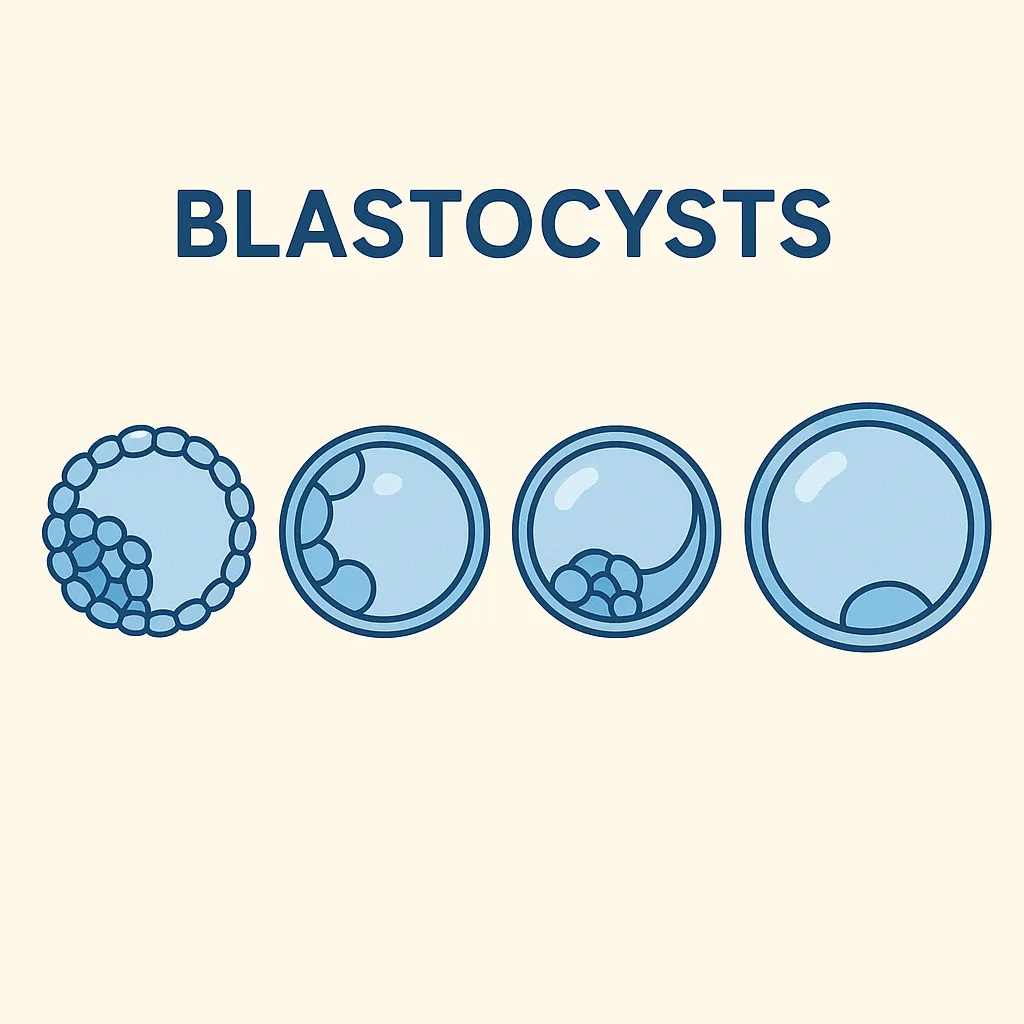
Example: Blastocyst Grading System
Expansion stage (1–6): Refers to how expanded the blastocyst is
Inner Cell Mass (ICM): Becomes fetus → graded A, B, or C
Trophectoderm (TE): Becomes placenta → graded A, B, or C
Example Grade: 5AA = highly expanded, excellent ICM, excellent TE
🔸 Note: Even lower-graded embryos (e.g., 4BC or 3BB) can result in healthy pregnancies.
🔹 Preimplantation Genetic Testing for Aneuploidy (PGT-A)
PGT-A tests embryos for chromosomal abnormalities (aneuploidy), helping select euploid (chromosomally normal) embryos.
How it works:
A few cells are biopsied from the trophectoderm on day 5–6.
DNA is analyzed for missing or extra chromosomes.
Only euploid embryos are prioritized for transfer.
When PGT-A is Recommended:
Age > 35
Recurrent miscarriage
Repeated IVF failure
Male factor infertility
Pros:
Higher implantation and lower miscarriage rates
Informs transfer decision (especially with multiple embryos)
Controversies:
Mosaic embryos (part normal, part abnormal) may be viable but are often discarded.
A biopsy may not represent the whole embryo, especially in early stages.
Adds cost and complexity to treatment
✅ Summary Table
IVF Decision Point Standard Today Embryo Freezing Vitrification of blastocysts Number of Embryos Transferrede SET for most patients under 38Selection Method Embryo grading + optional PGT-A Goal One healthy baby at a time