The Evolution of Medications in IVF: From the 1970s to Today
Introduction
Since the birth of Louise Brown in 1978, the world's first IVF baby, in vitro fertilization has transformed from an experimental procedure to a mainstream fertility treatment. Alongside advances in laboratory techniques and cryopreservation, one of the most dramatic evolutions has been in the medications used to stimulate the ovaries and prepare the body for embryo transfer. This article explores how ovarian stimulation protocols have evolved—from the rudimentary drug regimens of the 1970s to the sophisticated protocols used in modern IVF cycles.
IVF in the 1970s: The Early Days of Ovarian Stimulation
In the earliest days of IVF, physicians worked with a limited pharmacologic toolkit. The goal was to induce ovulation or retrieve a single oocyte naturally—far from today’s multi-oocyte retrievals.
Key Medications Used:
Clomiphene Citrate (Clomid®):
Approved by the FDA in 1967, Clomid was among the first fertility drugs used in early IVF. It works as a selective estrogen receptor modulator (SERM), blocking estrogen receptors in the hypothalamus and triggering an increase in FSH (follicle-stimulating hormone) secretion. In the late 1970s, it was used primarily for minimal stimulation protocols or natural cycles.Human Chorionic Gonadotropin (hCG):
Urinary-derived hCG (like Pregnyl®) was used to mimic the luteinizing hormone (LH) surge and trigger final oocyte maturation before retrieval. It remains a cornerstone in today’s protocols.Natural Cycles:
In many of the earliest attempts, IVF cycles were conducted without stimulation. Physicians would monitor a woman’s natural ovulation cycle and retrieve a single egg. This limited egg quantity and cycle control but was necessary due to the limited drugs available and concerns over ovarian hyperstimulation.
1990s–Early 2000s: Advancing the Science with Gonadotropins and GnRH Analogues
As IVF success rates increased, clinicians began using more aggressive stimulation to retrieve multiple oocytes per cycle, improving fertilization chances.
Additions to the Protocol:
Urinary Gonadotropins (hMG, FSH):
Human menopausal gonadotropin (hMG) such as Menopur® provided both FSH and LH activity. Pure urinary FSH (uFSH), like Bravelle®, became available in the 1990s.GnRH Agonists (e.g., Lupron®):
Introduced to prevent premature LH surges, agonists initially overstimulate then suppress pituitary gonadotropin release. These long protocols allowed better control over the cycle.
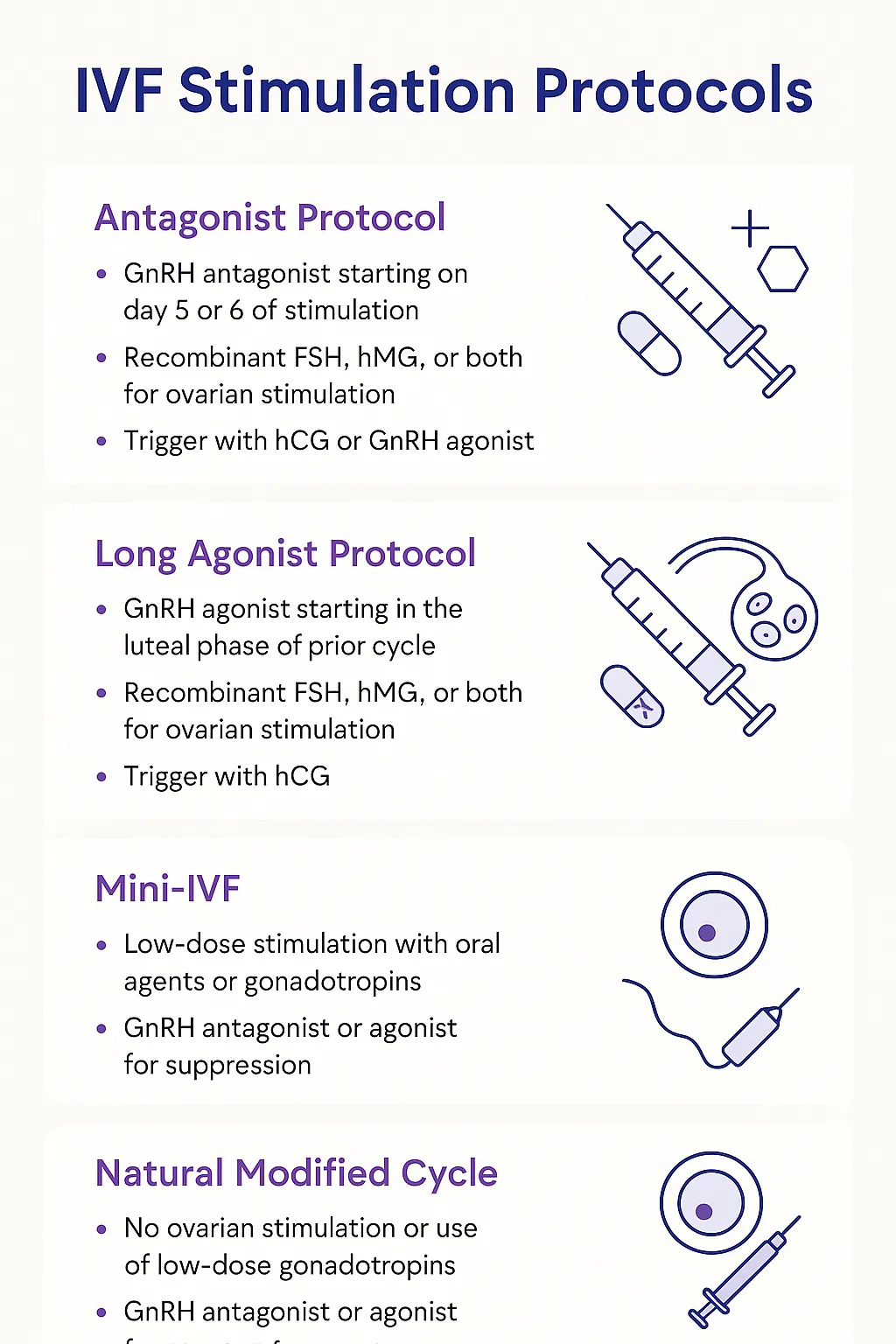
Modern IVF (2010s–Today): Tailored Protocols with Recombinant Technologies and Antagonists
Today’s IVF protocols offer a customized approach based on the patient’s ovarian reserve, age, and treatment goals. Physicians now have a wide range of pharmaceutical tools, most of them recombinant and highly purified.
Modern Medications Include:
Ovarian Stimulation:
Recombinant FSH (rFSH):
Examples: Gonal-F®, Follistim AQ®
These are lab-manufactured and more consistent than urinary versions.
hMG / Menopur® (FSH + LH):
Still used, especially for patients with low LH or advanced maternal age.
Cycle Control:
GnRH Antagonists (e.g., cetrorelix [Cetrotide®], ganirelix):
Quickly suppress LH surge without the downregulation phase needed in agonist protocols.
Ovulation Trigger:
hCG (Pregnyl®, Novarel®) or Recombinant hCG (Ovidrel®)
GnRH Agonist Trigger (for antagonist cycles):
Used to reduce OHSS risk in high responders (e.g., Lupron® trigger).
Luteal Phase Support:
Progesterone (IM injections, vaginal gel/suppositories):
Progesterone support is universal after embryo transfer.
Adjuvants (in select patients):
Letrozole or Clomid® (in mild stimulation)
Low-dose aspirin, prednisone, or intralipids (for implantation failure or immune issues)
Growth hormone or DHEA (for poor responders)
Looking Ahead
As IVF enters an era of precision medicine, new research focuses on optimizing ovarian response, minimizing side effects, and maximizing egg quality. Advances such as long-acting FSH formulations, micro-dose regimens, and biosimilar gonadotropins continue to reshape how stimulation is approached.